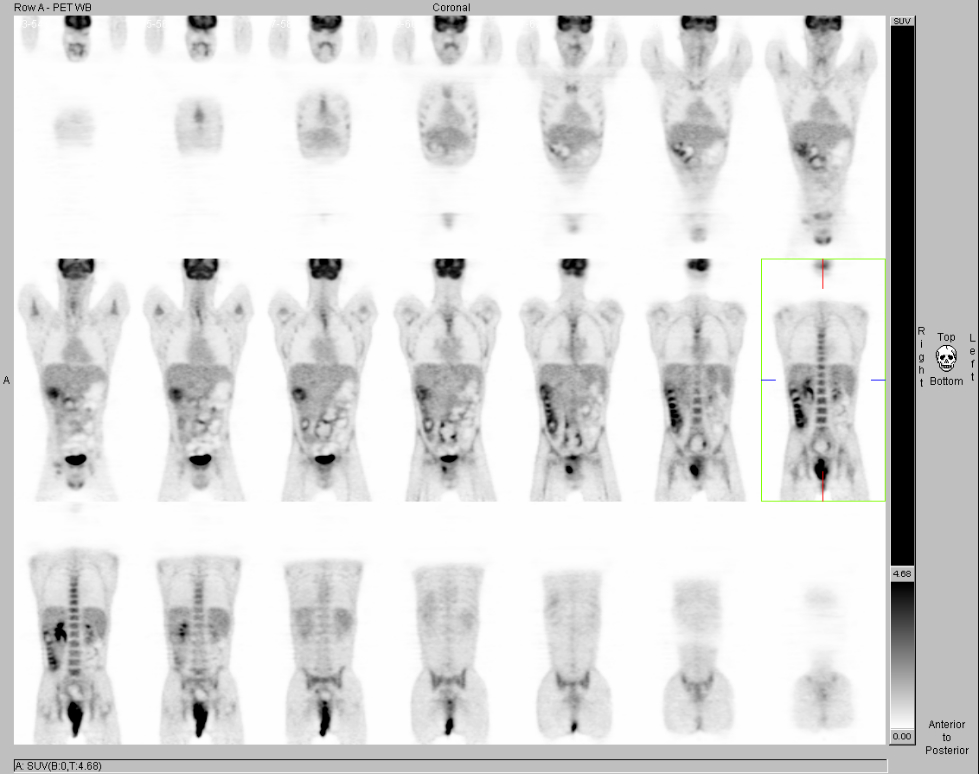
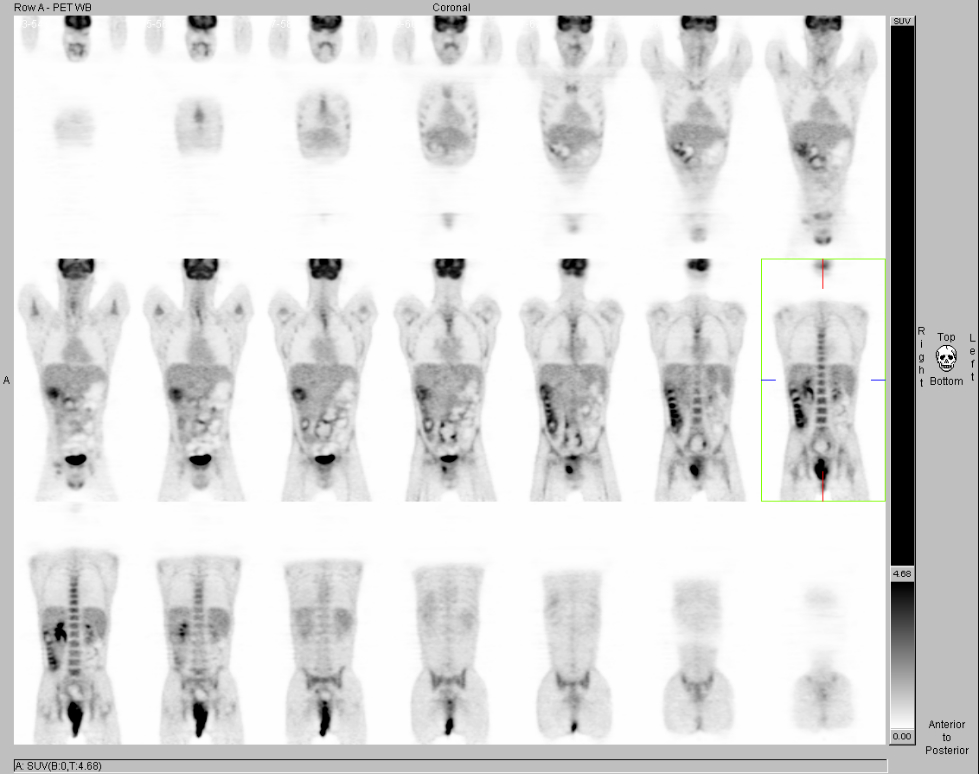
Coronal FDG-PET images.
View main image(pt) in a separate image viewer
View second image(pt). Axial FDG-PET images.
View third image(pt). Axial PET/CT images.
View fourth image(). Axial CT with contrast at the level of upper thighs.
Full history/Diagnosis is available below
Incidental note is made of a large amount of retained barium within the dilated colon and dilated small bowel from oral contrast administration of abdominal CT one month ago, and is suggestive of bowel obstruction.
There is increased FDG uptake in bone marrow. This is consistent with anemia.
Spread of anal cancer is mainly local and regional. Anal muscles are invaded early because the mucosa is very close to the underlying sphincters. The growth of anal canal cancer is circumferential, a characteristic that produces narrowing and stenosis of the anal sphincter. When the sphincter is invaded, the tumor spreads into the ischiorectal fossae, the prostatic urethra and bladder in men, and the vagina in women. Anal canal caner may spread via the lymphatic vessels to the perirectal nodes or at a higher level, to nodes at the bifurcation of the superior rectal artery. Hematogenous spread of anal canal cancer develops in fewer than 10% of cases. Liver metastasis is more common than lung or bone metastasis and usually occurs in the case of a tumor arising at the anorectal junction.
The primary tumor may be directly visualized as a hypoattenuated necrotic mass on a contrast enhanced CT scan. Unfortunately, the tumor may be isoattenuated with respect to the musculature. In such cases, the presence of the lesion can only be suspected from indirect signs (1) symmetric bulging of the sphincter or levator ani muscles in cases of supralevator masses, (2) asymmetry of the perirectal fat between the anorectal walls and levator ani, (3) asymmetry in the thickness of the sphincter or levator ani muscles of the two sides, (4) linear stranding in the perirectal fat or upper ischiorectal fossa.
The goals of therapy in patients with malignant anal canal tumors are to ablate the neoplasm and to preserve anal sphincter function. Excellent results can be obtained with a combination of radiation therapy and chemotherapy without surgical intervention.
The PET/CT has become a useful imaging modality in initial staging a variety of cancers and treatment response. In the initial staging and post treatment restaging of patients with anal cancer, PET/CT imaging plays an important role in the assessment of disease following therapy. Anal cancer frequently responds dramatically to chemoradiation with marked reduction in size and maximum SUV after effective treatment. A residual mass after therapy and the differentiation between residual viable anal cancer and post-treatment necrosis and fibrosis is a big challenge with CT imaging. PET/CT helps determine whether additional therapy is need. In particular, PET/CT is very powerful in accurate localization of small anal tumor less than 2 centimeters that would be very difficult or not possible to localize on CT scan alone.
Reference:
Radin DR. Squamous cell carcinoma of anus and rectum in homosexual men: CT findings. J Comput Assist Tomogr. 1994 Nov-Dec; 18(6):921-4
Daling JR, Weiss NS, Hislop TG, et al. Sexual practices, sexually transmitted disease, and the incidence of anal cancer. N Engl J Med 1987;317:973-7
Antoine Scherrer, Francois Roboul, et al. CT of Malignant Anal Canal Tumors. RadioGraphics 1990; 10:433-453
Thomas G. Trautmann, James H. Zuger. Positron Emission Tomography for Pretreatment Staging and Posttreatment Evaluation in Cancer of the Anal Canal. Mol Imaging Biol(2005) 0:1-5
View followup image(pt). Partial response of extensive anal carcinoma to radiation and chemotherapy with interval decrease in tumor size and FDG uptake in comparison with the prior study of 6-22-05. The increased activity seen could potentially represent tumor, residual infection, or post-radiation-inflammation, or mixtures of the above.
References and General Discussion of PET Tumor Imaging Studies (Anatomic field:Gasterointestinal System, Category:Neoplasm, Neoplastic-like condition)
Return to the Teaching File home page.