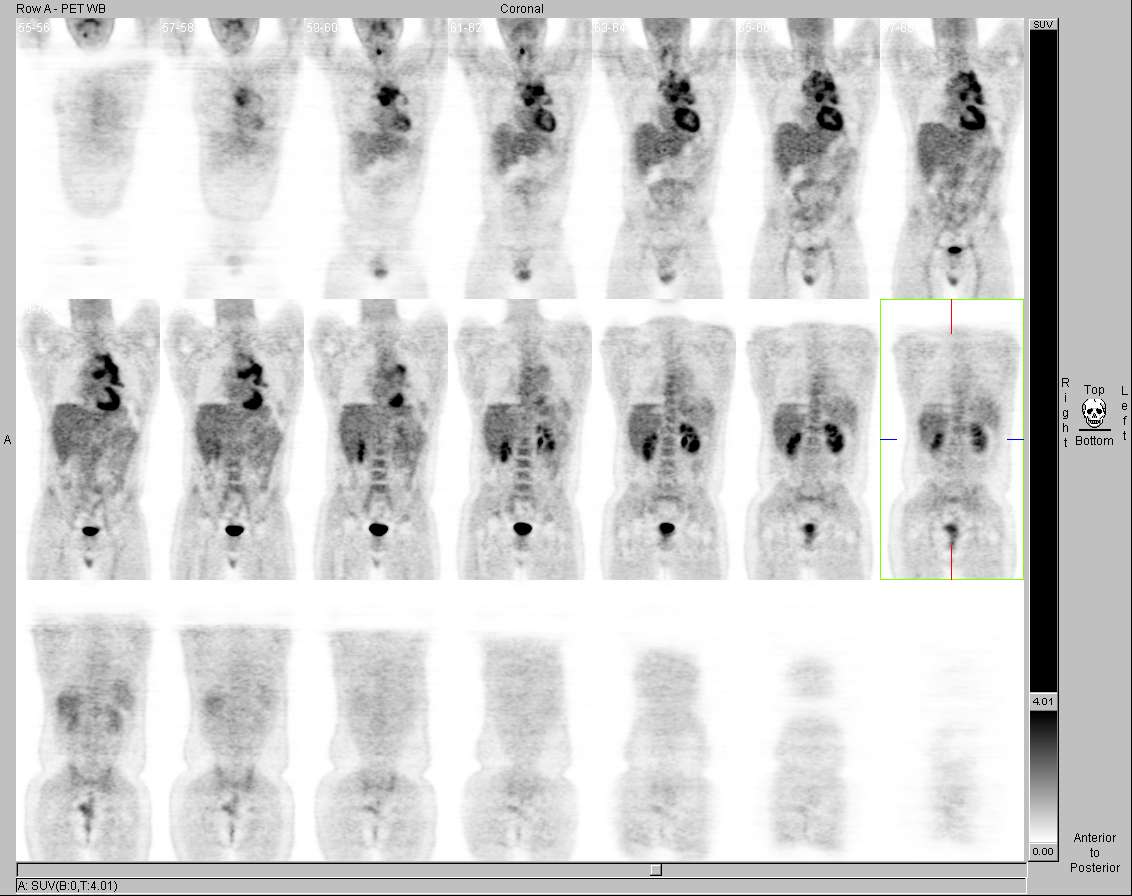
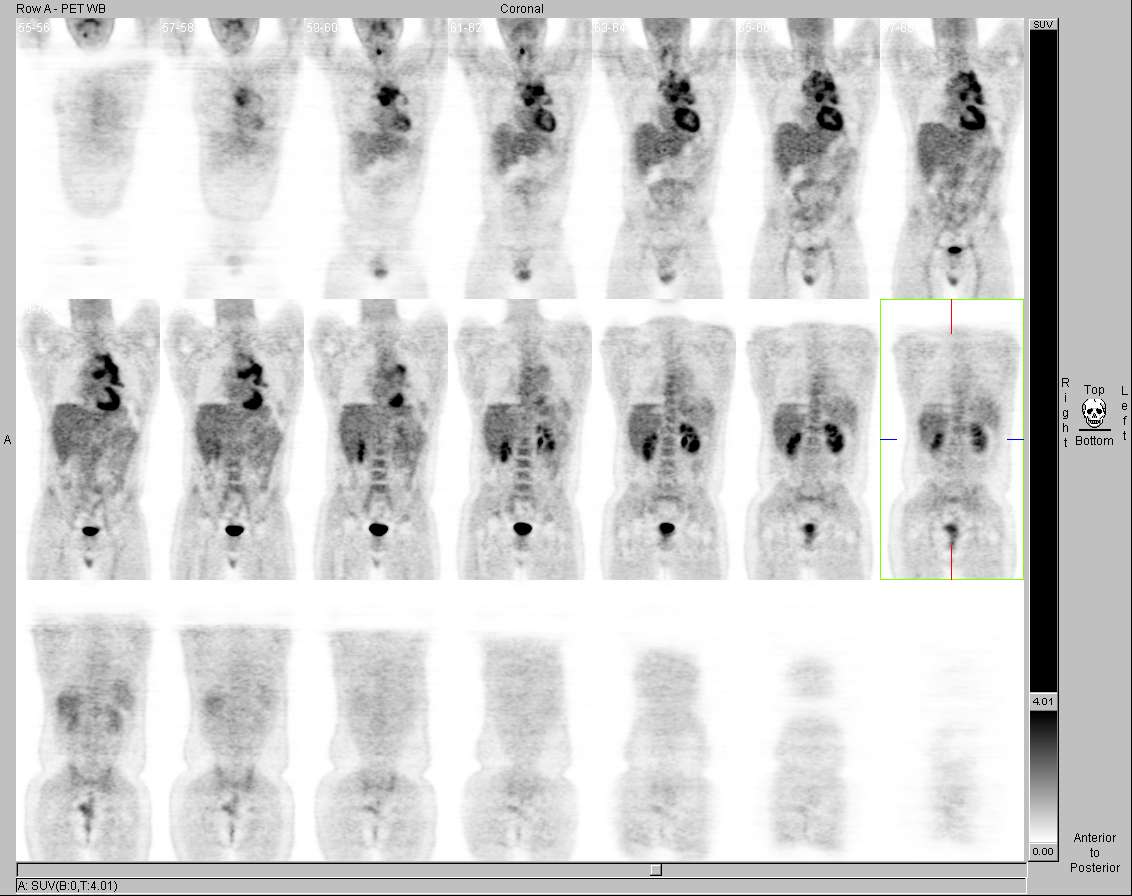
Coronal FDG-PET images. View MIP cine in AVI format.
View main image(pt) in a separate image viewer
View second image(pt). Axial FDG-PET/CT images.
View third image(pt). Axial PET/CT images.
View fourth image(pt). Axial CT image.
Full history/Diagnosis is available below
There is asymmetrically increased FDG uptake involving the right vocal cord with lack of FDG uptake within the left vocal cord. This is most likely secondary to left vocal cord paralysis from compression of the left recurrent laryngeal nerve by this bulky mass.
The CT portion of the examination demonstrates that the left vocal cord is collapsed and also shows a pericardial effusion.
Symmetrically increased FDG uptake in the vocal cords and muscles of phonation is often seen in patients who talk during the FDG uptake phase of the examination; this is a normal variant, due to the increased glucose utilization of these active muscles. The finding of asymmetric FDG uptake in the laryngeal muscles warrants investigation, to determine if the side with increased activity harbors a tumor or if the side with relatively decreased uptake is a result of vocal cord paralysis secondary to a mass lesion along the course of the recurrent laryngeal nerve or as a result of injury during surgery (e.g., thyroidectomy) or radiation therapy.
The differential diagnosis of an anterior mediastinal mass includes thymic tumors, germ cell tumors, lymphoma (and other causes of lymphadenopathy), and thyroid masses.
Hodgkin’s lymphoma occurs with a bimodal age distribution, with peaks at 30 and 70 years. Radiographic features include superior mediastinal nodal involvement, contiguous progression from one lymph node group to next, 15% lung involvement, 15% pleural effusion.
Most (85 %) Non-Hodgkin’s lymphomas arise from B cells and the remainder (15%) arise from T cells. 60% originate in lymph nodes and 40% in extranodal sites. There is an increased incidence in patients with altered immune status, including patients post transplantation and those with AIDS, congenital immunodeficiency syndomes, and collagen vascular disease (RA, SLE). Radiographic features are generalized or noncontiguous mediastinal and hilar adenopathy, lung involvement, extrathoracic spread( nasopharynx, GI tract, spread to unusual sites).
Thymoma is the most common anterior mediastinal tumor in adults. 30% are invasive. 35% of patients have myasthenia gravis. Radiographic features include asymmetrical location on one side, homogenous density and signal intensity; some have cytic components and contrast enhancement. Invasive thymomas show growth beyond the capsule into adjacent tissues. Drop metastases into the pleural space are common. 20% presents with a calcified mass.
Multinodular goiter is the most common thyroid mass that extends into the mediastinum. Radiographic features include thoracic inlet masses, contiguous with the cervical thyroid gland, heterogenous density by CT, and marked and prolonged contrast enhancement on CT.
Germ cell tumors include seminoma, embryonal cell carcinoma, choriocarcinoma, teratoma and yolk sac tumor. 70% of germ cell tumors are teratomas. Teratoma typically presents as a large mass lesion with variable tissue contents (calcification, fat, fat-fluid levels, cystic areas, soft tissue).
View followup image(pt). Another PET/CT images to demonstrate the tumor.
References and General Discussion of PET Tumor Imaging Studies (Anatomic field:Lung, Mediastinum, and Pleura, Category:Neoplasm, Neoplastic-like condition)
Return to the Teaching File home page.